Sarah Mount
Impact of COVID-19 on the Medical Industry
COVID-19 is a virus that has had a huge effect on every country on Earth. It originated in China around the end of 2019 and there have been about 46.6 million cases. Out of those cases, 31.2 million people have recovered, but over 1.2 million people have died (Linnane). The disease spreads very easily and quickly, which makes it hard to contain. The people most affected by COVID-19 are people in the medical industry. They are on the front lines, treating people with the virus and putting themselves and their families at higher risk. We have also seen an increase in everyday people wearing some form of personal protective equipment in order to do their part in slowing the spread of COVID-19. Even with more measures being put in place to slow the spread of the virus, COVID-19 to spread. Because of this, we have seen a rapid increase in medical technology development during the times of COVID-19.
Connection to STS Theory
Actor- Network Theory
Actor-Network Theory is the idea that anything that happens is a result of interactions between people or things, aka actors. These interactions are all connected and shape what is happening in a certain way, creating a network. COVID-19 ’s effects on medical technology is a great example of the Actor-Network Theory. You have people, COVID-19, and technology as actors and the way they interact becomes the network. People are interacting with other people or not interacting for the sake of social distancing, by delivering groceries or similar things to those who are at high risk and can’t go out. There are also interactions between people and COVID-19 as people get the virus or try to protect themselves from it. The biggest interaction is probably between people and technology. During this time there is a greater need for technology than ever. This is especially the case in the medical field, where staying out of direct contact with the virus can be difficult because of the close proximity between health workers and their patients. All these interactions have created a larger network for everyone and everything is being affected by COVID-19 .
Telemedicine and Personal Protective Equipment
One of the things that COVID-19 does best at is spreading. It spreads so fast that at one point the only way to even slow it down was to have everyone self quarantine and stay home for a few months. The contagiousness of COVID-19 puts medical professionals at the most risk. They could see hundreds of patients in a single day and the odds that at least one of those patients is COVID-19 positive is very high. That is why telemedicine, or virtual medicine, has been so important during this pandemic. Telemedicine helps to promote social distancing measures. It also help medical centers avoid prolonged waiting times and risk of disease progression (Bokolo). Doctors could now see patients over the computer which cut down the amount of people they would have to be physically near. The biggest issue with telemedicine was “Only a few physicians and patients are adequately educated on how best practice on how to utilize these digital services” (Bokolo). There was a huge learning curve when it came to trying to see patients virtually. Doctors did improve with time. As they saw more and more patients they got better at using online communications programs. Telemedicine also got easier as everyday people started getting used to having meetings online.

Not only was telemedicine useful. So is the use of personal protective equipment. While telemedicine is great for smaller doctor offices or clinics it isn’t really useful for doctors and nurses who are treating actual COVID-19 patients. Their best line of defense is personal protective equipment (PPE). This includes gloves, face masks and shields, and anything else they may use to protect themselves from the virus. Northwestern University is working on what some have called smart PPE (Farabaugh). What they are making can be described as face masks with tiny sensors in them that can detect all kind of things, from symptoms of COVID to fatigue. Such sensors can even detect issues such as if a mask fits a person’s face or if they are wearing it properly (Farabaugh). This would be a huge benefit to physicians treating people with the virus because it allows them to do so in a safer manner. Smart PPE also gives them peace of mind that they are wearing their equipment properly, reducing their worries about becoming infected and making them more focused on treating patients. Safer PPE also prevents doctors from spreading the virus when they are in or out of the hospital. It also isn’t just medical professionals who wear some kind of personal protective equipment.
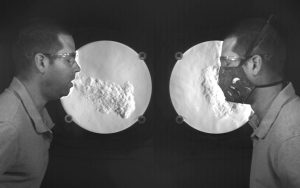
Another key way to slow and stop the spread of COVID-19 is for everyday people to also wear face masks. These face masks are different from the ones medical professionals wear. They are usually simple cloth face coverings. Many people are making and selling homemade cloth masks that can be washed and reused instead of using new surgical masks, which have to be thrown out after each use. There are some people who think that we shouldn’t have to wear masks in public. They believe that it doesn’t do anything to slow the spread of the virus. There are also people who will wear masks but pull them down under their nose, which defeats the whole purpose of wearing the mask. The National Institute of Standards and Technology came out with an experiment that shows airflow when wearing masks. Scientists who conducted the experiment wore different types of masks and coughed or sneezed in front of a high speed camera that can show airflow. The study found that “A good seal around the nose, chin and cheeks helps to prevent your cough from ’leaking’ out of the covering. And pulling your face covering below your nose is not good — you would be surprised how much air comes out of your nose when you cough. Additionally, we found that fabrics with very tight and nonporous weaves actually increase air leaking out by the nose and chin. So, while these tight fabrics may filter droplets at a greater efficiency, they are not breathable and could possibly defeat the purpose of the face covering” (Staymates). This is great information to know because many people are making and selling these masks.
Medical Innovation
Another thing that has come out of COVID-19 was a huge wave of innovation. People took everyday objects and found ways to use them to help others who were very sick due to the virus. In Spain, a shortage of ventilators led a group of engineers to use a car windshield wiper motor to make a respiration bag function (Naumova). In France, a former physician used a design for a snorkeling mask and other 3D printed parts to create a continuous positive airway pressure mask (Naumova). These masks then would connect to an oxygen supply and were a viable option if hospitals ran out of the actual masks. There was also a hackathon in Germany. Over 42,000 people worked together on different problems concerning COVID-19, such as contract tracing, border controls, and how to get people to stay at home (Naumova). People have really come together to help those affected by COVID-19 and try to find ways to solve the major problems the pandemic has created. Still, the best way to fight the virus is to come up with a vaccine.
Many companies are trying to create a vaccine for COVID-19. The hardest part is simply the time frame. It can take years to come up with a vaccine that we know is safe just because of all the testing involved. The last thing that people want to happen is 10 or 20 years down the line there is some huge side effect that harms everyone who got vaccinated. One of the companies trying to tackle this problem is Voltron Therapeutics. They are working with Hoth Therapeutics to create a vaccine. The two companies are using “a platform developed at MGH called VaxCelerate, which is designed to quickly generate and test “self assembling” vaccines that spark immune responses to viruses. The experimental COVID-19 vaccine uses a heat shock protein to activate the immune system, rather than one of the chemical adjuvants that are commonly employed by vaccine developers, the company said” (Weintraub ). These vaccines would be easy to change in case there was a shift in the genetic makeup of the virus.

In China, a few scientists performed a survey on the effect of technology on limiting the spread of COVID-19. They looked at how their government responded to the virus and how much this response depended on technology. A new technology that had a huge impact on limiting the disease was a health QR code. The QR codes, according to the study, “played an important role in epidemic prevention and control as well as enabling people to return to work” (Ye et al.). Basically, people were required to show/scan their QR code when entered or left public places like supermarkets, restaurants, or transportation (Ye et al.). If someone was to test positive for COVID-19 then the government would be able to quickly retrace that person’s steps and do what was necessary to stop the spread of the virus (Ye et al.). QR code also had the effect of making people more accountable for their movements because they would be unable to go anywhere if they tested positive. People may say that that is an invasion of their privacy, but seeing how bad COVID-19 has been it might be what is necessary to be able to stop the virus from spreading even more than it already is.
Conclusion
Overall, technology has had a huge impact on how we fight against COVID-19. Compared to the Spanish Flu the current pandemic has been a cakewalk. COVID-19 has killed about 1.2 million people compared to the estimated 50 million people who died due to the Spanish Flu (Strickland & Zorpette). Technology we have today has allowed us to ramp up testing, diagnostics, modeling, treatment, vaccine creation and develop innovations in a very short time period. One of the biggest advantages we have is the ability to create a model of how the virus would impact us (Strickland & Zorpette). Knowing beforehand where COVID-19 was likely to hit the hardest allowed government officials to stock up on supplies and prepare for outbreaks in specific places. This pandemic has affected everyone. In response to that people all over the world responded, creating new inventions and innovations to fight back against COVID-19. If not for innovations in medical and other technology COVID-19 probably would have had an even worse impact and thousands more would probably be dead.
References
Bokolo, Anthony. “Use of Telemedicine and Virtual Care for Remote Treatment in Response to COVID-19 Pandemic.” Journal of Medical Systems, vol. 44, no. 7, 2020, pp. 132. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7294764/.
Farabaugh, Kane. “COVID-19 Sparks Technology Innovation.” Voice of America, 19 Jun. 2020, http://www.voanews.com/covid-19-pandemic/covid-19-sparks-technology-innovation. Accessed 1 Dec. 2020.
Linnane, Ciara. “Coronavirus tally: Global cases of COVID-19 46.6 million, 1.2 million deaths and Trump hints at firing Fauci.” MarketWatch, 2 Nov. 2020, https://www.marketwatch.com/story/coronavirus-tally-global-cases-of-covid-19-466-million-12-million-deaths-and-trump-hints-at-firing-fauci-2020-11-02. 1 Dec. 2020.
Naumova, Evgeniya. “How tech and innovation are fighting the coronavirus, Covid-19.” Secure Futures, 2020, http://www.kaspersky.com/blog/secure-futures-magazine/technologies-fighting-coronavirus/34626/. Accessed 1 Dec. 2020.
Staymates, Matthew. “My Stay-at-Home Lab Shows How Face Coverings Can Slow the Spread of Disease.” National Institute of Standards and Technology, 29 Jul. 2020, http://www.nist.gov/blogs/taking-measure/my-stay-home-lab-shows-how-face-coverings-can-slow-spread-disease. Accessed 29 Jul. 2020, July 29.
Strickland, Eliza and Glenn Zorpette. “Here’s How We Prepare for the Next Pandemic.” IEEE Spectrum, 30 Sep. 2020, https://spectrum.ieee.org/biomedical/devices/heres-how-we-prepare-for-the-next-pandemic. Accessed 30 Nov. 2020.
Weintraub, Arlene. “Researchers harness new technology for rapid COVID-19 vaccine development.” Fierce Biotech, 6 Apr. 2020, http://www.fiercebiotech.com/research/researchers-harness-new-technology-for-rapid-covid-19-vaccine-developmentfiercebiotech.com/…/researchers-harness-new-technology-for-rapid-covid-19-vaccine-development. Accessed 1 Dec. 2020.
Ye, Qing, et al. “Using Information Technology to Manage the COVID-19 Pandemic: Development of a Technical Framework Based on Practical Experience in China.” JMIR Medical Informatics, vol. 8, no. 6, 2020, pp. 19515, https://pubmed.ncbi.nlm.nih.gov/32479411/. Accessed 1 Dec. 2020.
Images
“COVID-19 Sparks Technology Innovation” by VOA News is in the Public Domain.
“My Stay-at-Home Lab Shows How Face Coverings Can Slow the Spread of Disease” by Matthew Staymates is in the Public Domain
“Citizens of Wuhan lining up outside of a drug store to buy masks during the Wuhan coronavirus outbreak” by China News Network is licensed under CC BY 3.0
